Options for Managing the Menopause and Peri Menopause for Women who have had Breast Cancer
Women who have had breast cancer can sometimes feel that their options for managing menopause and peri menopause symptoms are limited, and it can be disappointing or confusing trying to understand the choices these women have.
There are different types of breast cancer and treatments. This will influence what your choices are for treating any menopausal symptoms. Other factors to consider when talking to your doctor is how long ago your diagnosis was, whether you are taking any treatment to reduce to risk of recurrent disease, how severe and what your symptoms are. So, there are quite a lot of particular points about each individual that needs to be considered. This includes your priorities and aims for your life now and your future.
Some women with a history of breast cancer will decide to take HRT. This is not the first line choice for women usually and this decision would be made after through discussions with your doctor, oncologist and breast team.
In this article I am going to discuss the treatment options for women who have chosen not to take HRT and would like guidance on other ways to improve menopause symptoms.
If hot flushes are a symptom that needs addressing, there are several medications which can be prescribed, they have a primary use for certain conditions, but as a side effect can help reduce hot flushes. Overall studies show these medications can reduce hot flushes by 40-60%. These medications include: oxybutynin, gabapentin, pregabalin and some antidepressant medications e.g. venlafaxine and citalopram. Fluoxetine and paroxetine are antidepressants which can be taken to help hot flushes, but these should not be taken if someone is also taking tamoxifen. These medications have some side effects which can lead to women stopping them.
There are non-hormonal treatments which are available without a prescription. Currently there is a lack of evidence for these treatments in terms of effectiveness. However, some women may feel some benefit. These include ‘Femal’ or ‘Femarelle’; sage, vitamin E and Evening of Primrose. I would always advise to check that any over the counter products have the ‘Traditional Herbal Registration’ certification mark which guarantees that it has met certain defined standards.
CBT 'cognitive behavioural therapy’ has been used for hot flushes, low mood and other menopausal symptoms. There are studies to support it’s effectiveness at reducing the stress and bothersomeness associated with menopausal symptoms.
Relaxation and mindfulness can help make symptoms of the menopause more manageable. Hypnosis has some evidence to back up its potential benefit in reducing hot flushes and the associated symptoms. However, access to hypnosis targeting menopause symptoms is limited.
Some women have found acupuncture or reflexology helps their menopause symptoms. There is not clinical data to support the effectiveness of either of these treatments. But this does not mean in individual will not benefit.
There are triggers of menopausal symptoms which can be avoided. Everyone is different in terms of what triggers their symptoms. Common ones to be aware of are: spicy food, caffeine, alcohol and stress. Avoiding any triggers to symptoms can help.
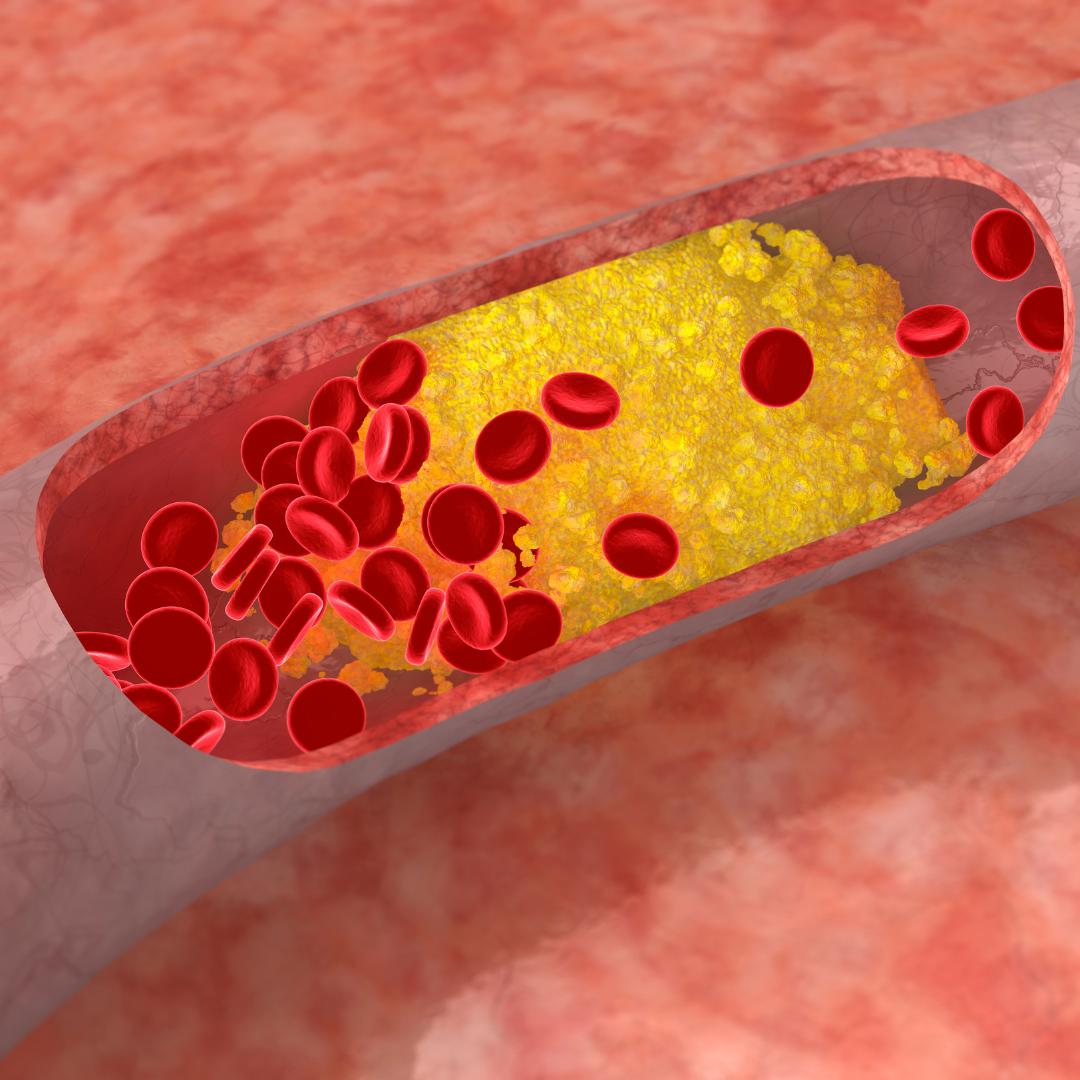
Making time to take care of yourself is important. Considering diet, exercise, sleep and ‘down time’. Staying active supports your bone and heart health and mental health. The power of moving your body cannot be underestimated. High stress levels can make every menopause symptom worse. A good balanced diet which avoids swings in blood sugars is very beneficial for overall health and can help many menopause symptoms.
Support from others can reduce stress and make symptoms more manageable. Talk with friends or find a supportive group who can empathize and provide comfort and understanding. There are such groups such as Harley Street at Home. Facebook and Instagram also have groups with the ability to interact with like minded people.
Vaginal and vulval oestrogen are an option for most women who have had breast cancer. These are called topical oestrogens, and are not ‘HRT’. They can be a tablet, pessary or ring which is placed into the vagina. Or a cream or gel applied to the vulva and vagina. They can be very effective for vaginal, vulval and urinary symptoms. The amount of oestrogen which gets absorbed into the blood stream as very small. Women taking aromatase inhibitors e.g. letrozole or anastrozole should not take these topical oestrogens. But women on tamoxifen can. Most of the evidence indicates topical oestrogen will not increase risk of recurrent breast cancer. I would always advise to discuss this with a doctor with knowledge in this area in order to weigh up the pros and any potential cons of using local oestrogen.
Vaginal moisturizers and lubricants can help comfort with sex and relieve vaginal dryness and itching. Not all brands are made with the health of the female genital region in mind. The best brands are ‘Yes’ and ‘Sylk’.
Testosterone replacement may be an option for some women with a history of breast cancer. Testosterone replacement can improve libido, low mood, cognitive functioning, motivation and energy. There is not enough evidence currently which addresses the safety or efficacy of testosterone only replacement with a history of breast cancer, leading to uncertainty in this area. A woman would need to be explore this thoroughly with a menopause specialist, the breast and oncology team.
Phytoestrogens such as Red Clover and Black Cohosh are not recommended to be used if there has been a history of breast cancer because they are structurally related to oestrogen.
There are many ways of targeting menopausal symptoms which does not involve using systemic HRT. Every women is individual in terms of disease history, prioritises, symptoms and goals. Many women who do not take HRT will benefit from trying more than one way of managing their symptoms.
Find more blogs like this:
www.harleystathome.com | Instagram @harleystreetathomemenopause
Facebook: Search Harley Street at Home: Diagnosis, Symptoms & Treatments or Harley St at Home: Lifestyle, Self-Care and Lifestyle to join our private community